Diabetes Survival Tips: Essential Strategies for Managing Your Blood Sugar and Living Well
Living with diabetes can feel overwhelming, particularly after initial diagnosis. However, understanding how to manage blood sugar levels, adopt healthy lifestyle habits, and prevent complications transforms diabetes from a frightening diagnosis into a manageable chronic condition. This comprehensive guide provides essential diabetes survival tips that help you maintain stable blood sugar, prevent complications, and enjoy quality of life. Whether you have Type 1 diabetes, Type 2 diabetes, or prediabetes, these practical strategies empower you to take control of your health through informed decisions and consistent daily habits.
Understanding Diabetes: The Foundation for Survival
Diabetes is a chronic condition affecting how your body processes blood glucose (sugar). Your body needs glucose for energy, but too much glucose in the bloodstream damages organs and tissues over time. According to the World Health Organization (WHO), diabetes is a major cause of blindness, kidney failure, heart attacks, stroke, and lower limb amputation globally.
Furthermore, the Ministry of Health Singapore recognizes diabetes as a significant health concern, with prevalence increasing in Singapore’s population. Therefore, understanding diabetes and implementing survival strategies becomes crucial for protecting long-term health.
Types of Diabetes You Need to Know
Understanding which type of diabetes you have helps guide appropriate management strategies:
Type 1 Diabetes: An autoimmune condition where the body produces little or no insulin. Consequently, people with Type 1 diabetes require insulin injections or pump therapy for survival. This type typically develops in childhood or young adulthood, though it can occur at any age.
Type 2 Diabetes: The most common type, occurring when the body becomes resistant to insulin or doesn’t produce enough insulin. Type 2 diabetes often develops gradually and is strongly linked to lifestyle factors including obesity, poor diet, and lack of physical activity. Moreover, this type can often be managed through lifestyle changes, oral medications, or insulin when needed.
Prediabetes: A condition where blood sugar levels are higher than normal but not yet high enough for diabetes diagnosis. Importantly, prediabetes represents a critical warning that allows intervention to prevent or delay Type 2 diabetes development.
Gestational Diabetes: Diabetes developing during pregnancy that usually resolves after childbirth. However, women with gestational diabetes have increased risk for Type 2 diabetes later in life.
Why Blood Sugar Control Matters
Maintaining blood sugar within target ranges prevents both short-term and long-term complications. In the short term, uncontrolled blood sugar causes symptoms like excessive thirst, frequent urination, fatigue, and blurred vision. Over time, high blood sugar damages blood vessels and nerves throughout the body, leading to serious complications affecting eyes, kidneys, heart, and extremities.
Therefore, diabetes survival depends on consistent blood sugar management through the strategies outlined in this guide.
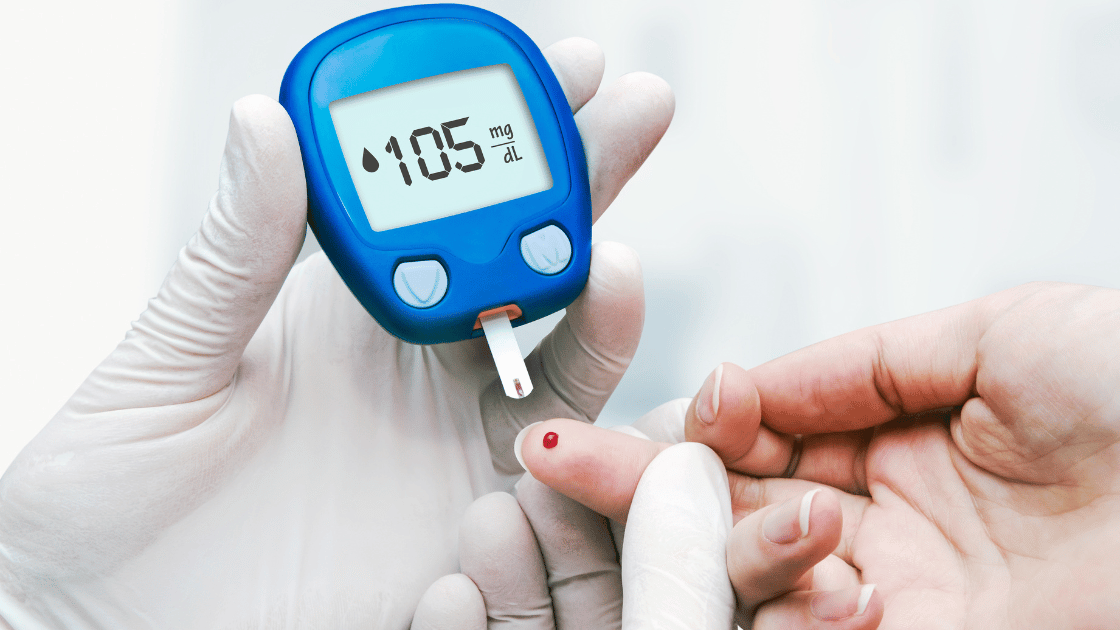
Survival Tip 1: Monitor Your Blood Sugar Regularly
Regular blood sugar monitoring represents the foundation of diabetes management. Understanding your blood sugar patterns helps you make informed decisions about food, activity, medication, and lifestyle.
Why Monitoring Matters
Blood sugar monitoring provides immediate feedback about how your body responds to different foods, activities, medications, and stressors. Consequently, monitoring allows you to identify patterns, catch problems early, and adjust management strategies before complications develop. Moreover, regular monitoring helps you understand your individual diabetes patterns rather than relying on general guidelines alone.
How to Monitor Effectively
Blood Glucose Meters: Traditional fingerstick testing provides accurate blood sugar readings. Most people with diabetes check blood sugar multiple times daily, particularly before meals and before bed.
Continuous Glucose Monitors (CGM): These devices provide continuous blood sugar readings throughout the day and night. CGMs offer tremendous advantages by revealing blood sugar trends and alerting you to dangerous highs or lows.
Laboratory Testing: Regular HbA1c testing through health screening shows average blood sugar control over the previous 2-3 months. This test provides the big picture of diabetes management effectiveness.
HOP Medical Centre’s health screening packages include comprehensive diabetes testing including HbA1c, fasting glucose, and other assessments that provide complete understanding of your diabetes control.
Understanding Your Target Numbers
Work with your healthcare team to establish personalized blood sugar targets. Generally, targets include:
- Fasting blood sugar: 80-130 mg/dL
- Blood sugar 2 hours after meals: Less than 180 mg/dL
- HbA1c: Below 7% (or as recommended by your doctor)
However, targets vary based on individual factors including age, diabetes duration, complications presence, and overall health status. Therefore, discuss appropriate targets with your healthcare provider rather than relying solely on general guidelines.
When to Check Blood Sugar
Timing matters for effective monitoring:
Essential Testing Times:
- Before meals
- Before bed
- Before, during, and after exercise
- When you feel symptoms of high or low blood sugar
- Before driving
- When sick or stressed
Additionally, occasional middle-of-the-night checks help identify overnight blood sugar problems that daytime testing might miss.
Survival Tip 2: Master Your Diet and Nutrition
Diet profoundly impacts blood sugar control. What you eat, when you eat, and how much you eat all affect blood sugar levels. Therefore, mastering diabetes nutrition becomes essential for survival and thriving with this condition.
Understanding Carbohydrates
Carbohydrates have the most significant impact on blood sugar among all nutrients. Your body breaks down carbohydrates into glucose, which enters the bloodstream and raises blood sugar levels. Consequently, managing carbohydrate intake represents the cornerstone of diabetes nutrition.
Types of Carbohydrates:
Simple Carbohydrates: Found in sugar, candy, soda, and refined grains. These carbohydrates raise blood sugar quickly and dramatically, making them difficult to manage in diabetes.
Complex Carbohydrates: Found in whole grains, vegetables, legumes, and fruits. These carbohydrates raise blood sugar more gradually, providing better blood sugar control. Moreover, complex carbohydrates contain fiber, vitamins, and minerals that support overall health.
The Diabetes Plate Method
The plate method provides a simple approach to balanced diabetes meals:
Fill Half Your Plate: Non-starchy vegetables like leafy greens, broccoli, peppers, tomatoes, and cauliflower. These vegetables provide nutrients and fiber with minimal blood sugar impact.
Fill One Quarter: Lean protein such as chicken, fish, lean beef, tofu, or legumes. Protein helps you feel satisfied without significantly raising blood sugar.
Fill One Quarter: Carbohydrate foods including whole grains, starchy vegetables, or fruits. Limiting carbohydrates to one quarter of your plate helps control portions and blood sugar.
Add: A serving of dairy or dairy alternative if desired.
This visual guide simplifies meal planning without complicated calculations or measurements.
Foods That Help Control Blood Sugar
Certain foods particularly benefit diabetes management:
Fiber-Rich Foods: Vegetables, whole grains, legumes, and fruits slow glucose absorption, preventing blood sugar spikes. Aim for at least 25-30 grams of fiber daily.
Lean Proteins: Fish, poultry, lean meats, eggs, tofu, and legumes provide essential nutrients without raising blood sugar.
Healthy Fats: Nuts, seeds, avocados, olive oil, and fatty fish provide satiety and support heart health without affecting blood sugar.
Non-Starchy Vegetables: These can be eaten freely, providing nutrients, fiber, and volume to meals with minimal blood sugar impact.
Foods to Limit or Avoid
Some foods make diabetes management more challenging:
Sugary Beverages: Soda, sweetened tea, juice, and energy drinks cause rapid blood sugar spikes. Additionally, liquid sugar provides no satiety, making it easy to overconsume calories.
Refined Grains: White bread, white rice, and regular pasta raise blood sugar quickly compared to whole grain alternatives.
Fried Foods: High in unhealthy fats and calories, fried foods contribute to weight gain and insulin resistance.
Processed Snacks: Chips, cookies, crackers, and candy bars typically contain refined carbohydrates, unhealthy fats, and excessive calories.
High-Sugar Desserts: Cakes, pies, ice cream, and pastries cause significant blood sugar elevations.
Meal Timing and Consistency
When you eat matters almost as much as what you eat:
Eat Regular Meals: Skipping meals or going too long between meals can cause blood sugar fluctuations. Aim for consistent meal timing each day.
Don’t Skip Breakfast: Starting the day with a balanced breakfast helps prevent blood sugar problems throughout the day.
Plan Snacks Strategically: Small snacks between meals can prevent blood sugar from dropping too low, particularly if you take diabetes medications.
Watch Evening Eating: Large, late meals or bedtime snacks high in carbohydrates can cause overnight blood sugar elevations.
Survival Tip 3: Stay Physically Active
Physical activity represents one of the most powerful tools for diabetes management. Exercise helps your body use insulin more effectively, lowers blood sugar, supports weight management, and reduces cardiovascular disease risk.
How Exercise Helps Diabetes
When you exercise, muscles use glucose for energy, lowering blood sugar levels. Additionally, physical activity improves insulin sensitivity, meaning your cells respond better to insulin. These effects can last for hours after exercise, providing sustained benefits. Moreover, regular exercise helps with weight management, which particularly benefits people with Type 2 diabetes.
Types of Exercise for Diabetes
Different exercise types provide various benefits:
Aerobic Exercise: Walking, jogging, swimming, cycling, and dancing improve cardiovascular health and help manage blood sugar. Aim for at least 150 minutes of moderate-intensity aerobic activity weekly, spread across several days.
Resistance Training: Weight lifting, resistance bands, and bodyweight exercises build muscle mass. More muscle means more glucose uptake from the bloodstream. Include resistance training at least twice weekly.
Flexibility and Balance: Stretching, yoga, and tai chi improve flexibility, reduce injury risk, and provide stress relief. These activities complement aerobic and resistance training.
Exercise Safety for People with Diabetes
Exercise affects blood sugar, so safety precautions matter:
Check Blood Sugar: Test before, during (for prolonged activity), and after exercise. This monitoring helps you understand how different activities affect your blood sugar.
Time Exercise Wisely: Avoid exercising when blood sugar is too high (over 250 mg/dL with ketones present) or too low (below 100 mg/dL without preventive carbohydrates).
Carry Fast-Acting Carbohydrates: Keep glucose tablets, juice, or candy available to treat low blood sugar during or after exercise.
Stay Hydrated: Drink water before, during, and after physical activity. Dehydration can affect blood sugar levels.
Wear Proper Footwear: Good shoes protect feet, which are vulnerable to injury in people with diabetes.
Inform Others: When exercising with others, let them know you have diabetes and how to help if problems arise.
Starting an Exercise Program
If you’re currently inactive, start gradually:
Begin Slowly: Even 10-minute walks provide benefits. Gradually increase duration and intensity as fitness improves.
Choose Enjoyable Activities: You’re more likely to maintain activities you enjoy. Try different options to find what works for you.
Schedule Exercise: Treat physical activity like any important appointment, scheduling it into your daily routine.
Find Exercise Partners: Working out with others provides motivation, accountability, and social connection.
Consult Your Doctor: Before starting new exercise programs, particularly if you have complications or have been inactive, discuss plans with your healthcare provider.
Survival Tip 4: Take Medications as Prescribed
Many people with diabetes require medications to achieve target blood sugar levels. Taking medications correctly represents a crucial survival strategy that prevents complications and maintains health.
Understanding Diabetes Medications
Insulin: All people with Type 1 diabetes require insulin. Many people with Type 2 diabetes eventually need insulin as the condition progresses. Various insulin types work at different speeds and for different durations.
Metformin: Often the first medication prescribed for Type 2 diabetes, metformin reduces glucose production in the liver and improves insulin sensitivity.
Other Oral Medications: Multiple drug classes help manage Type 2 diabetes through various mechanisms including improving insulin secretion, reducing glucose absorption, or increasing glucose excretion.
Injectable Non-Insulin Medications: Some newer medications given by injection help control blood sugar without being insulin.
Medication Adherence Tips
Taking medications consistently and correctly maximizes their effectiveness:
Set Reminders: Use phone alarms, pill organizers, or medication reminder apps to ensure timely doses.
Understand Your Medications: Know what each medication does, when to take it, and potential side effects. Moreover, understand how medications interact with food and other drugs.
Don’t Skip Doses: Missing medications causes blood sugar fluctuations that increase complication risk.
Store Properly: Some medications, particularly insulin, require specific storage conditions. Follow storage instructions carefully to maintain medication effectiveness.
Refill Before Running Out: Don’t let prescriptions lapse. Set up automatic refills or reminders to reorder medications before they run out.
Communicate with Healthcare Providers: Report side effects, concerns, or challenges with medications. Often, adjustments or alternatives can address problems while maintaining blood sugar control.
When to Adjust Medications
Blood sugar patterns change over time due to various factors including weight changes, activity level changes, other illnesses, or natural diabetes progression. Therefore, medication needs change accordingly. Never adjust medications without consulting your healthcare provider, but recognize when patterns suggest need for changes:
Signs You May Need Adjustments:
- Frequent high or low blood sugar readings
- Blood sugar patterns that don’t respond to dietary and lifestyle interventions
- HbA1c not at target despite medication adherence
- Side effects interfering with quality of life
- Life changes affecting diabetes management
Regular health screening including HbA1c testing helps identify when medication adjustments may be needed.
Survival Tip 5: Manage Stress Effectively
Stress significantly affects blood sugar through multiple mechanisms. When stressed, your body releases hormones that increase blood sugar levels. Additionally, stress often leads to poor health behaviors including overeating, skipping exercise, and neglecting blood sugar monitoring. Therefore, stress management becomes an essential diabetes survival skill.
How Stress Affects Blood Sugar
During stress, your body produces cortisol and adrenaline, hormones that increase blood glucose to provide energy for the “fight or flight” response. While this response helped our ancestors survive immediate threats, chronic modern stress keeps these hormones elevated, causing persistently high blood sugar. Moreover, stress affects sleep quality, which also impacts blood sugar control and insulin sensitivity.
Stress Management Strategies
Multiple approaches help manage stress effectively:
Relaxation Techniques: Deep breathing, progressive muscle relaxation, and meditation activate the body’s relaxation response, counteracting stress hormones. Even 5-10 minutes daily provides benefits.
Regular Exercise: Physical activity reduces stress hormones and triggers endorphin release, improving mood and reducing anxiety. Furthermore, exercise provides a healthy outlet for stress-related energy.
Adequate Sleep: Aim for 7-9 hours nightly. Poor sleep increases stress hormones and makes blood sugar management more difficult.
Social Support: Connecting with family, friends, or support groups reduces stress and provides emotional support for diabetes management challenges.
Time Management: Organizing tasks and setting priorities reduces feeling overwhelmed. Break large tasks into smaller, manageable steps.
Professional Help: If stress, anxiety, or depression significantly impacts your life, consider working with a mental health professional. These conditions are common in people with chronic diseases and respond well to treatment.
Building Resilience
Beyond managing acute stress, building resilience helps you cope with diabetes challenges long-term:
Maintain Perspective: Diabetes management requires daily attention but doesn’t define you. Balance diabetes care with other life aspects that bring joy and meaning.
Celebrate Successes: Acknowledge progress and successes, no matter how small. Positive reinforcement supports continued healthy behaviors.
Learn from Setbacks: View challenges as learning opportunities rather than failures. Every person with diabetes experiences difficult days or weeks.
Stay Connected: Isolation increases stress and makes diabetes management harder. Maintain relationships and seek support when needed.
Practice Self-Compassion: Treat yourself with the same kindness you’d offer a friend facing similar challenges.
Survival Tip 6: Prevent and Detect Complications Early
Diabetes complications develop silently over years, causing damage before symptoms appear. Therefore, proactive monitoring and prevention strategies represent critical survival skills that protect long-term health.
Understanding Diabetes Complications
High blood sugar damages blood vessels and nerves throughout the body, potentially affecting:
Eyes: Diabetic retinopathy can cause vision loss or blindness. Regular eye examinations detect changes early when treatment prevents vision loss.
Kidneys: Diabetic kidney disease (nephropathy) progresses silently. Blood and urine tests detect early kidney damage before symptoms appear.
Heart and Blood Vessels: Diabetes significantly increases heart disease and stroke risk. Blood pressure and cholesterol management reduce cardiovascular complications.
Nerves: Diabetic neuropathy causes numbness, tingling, or pain, particularly in feet and hands. Nerve damage also affects digestion, bladder function, and sexual function.
Feet: Reduced blood flow and nerve damage make feet vulnerable to infections and injuries that heal slowly or lead to serious complications.
Prevention Through Good Control
The single most important complication prevention strategy is maintaining blood sugar, blood pressure, and cholesterol within target ranges. Studies consistently show that good control dramatically reduces complication risk. Therefore, daily management efforts pay off through preserved health and quality of life.
Recommended Screening Schedule
Regular screening detects complications early when treatment is most effective:
Annual Comprehensive Foot Examination: Check for sensation loss, circulation problems, and skin issues. Additionally, examine feet daily at home for any cuts, blisters, or changes.
Annual Eye Examination: Dilated eye exam by an eye specialist detects diabetic retinopathy early. More frequent exams may be needed if retinopathy is present.
Regular Kidney Function Testing: Annual urine tests (for protein) and blood tests (for kidney function) detect kidney damage early.
Regular Blood Pressure Checks: Monitor blood pressure at each healthcare visit, or more frequently if elevated.
Annual Cholesterol Testing: Lipid panels assess cardiovascular disease risk.
HbA1c Testing: Check every 3-6 months to monitor overall blood sugar control.
HOP Medical Centre’s executive health screening packages include comprehensive diabetes monitoring with HbA1c testing, kidney function assessment, lipid profiles, and other tests that detect complications early.
Daily Self-Care for Prevention
Beyond medical screening, daily self-care prevents complications:
Foot Care: Inspect feet daily, wash and dry thoroughly, moisturize (but not between toes), wear proper footwear, and never go barefoot. Report any cuts, blisters, or changes to your healthcare provider immediately.
Dental Care: Brush teeth twice daily, floss daily, and see your dentist regularly. Diabetes increases gum disease risk, which worsens blood sugar control.
Skin Care: Keep skin clean and moisturized. Inspect skin regularly for cuts, sores, or infections that need attention.
Blood Pressure Monitoring: If you have high blood pressure, monitor at home between medical visits.
Survival Tip 7: Know When Blood Sugar Is Too High or Too Low
Recognizing and responding to blood sugar extremes prevents dangerous situations and helps you maintain better overall control.
Hyperglycemia: High Blood Sugar
Hyperglycemia occurs when blood sugar rises too high, typically above 180 mg/dL after meals or 130 mg/dL before meals.
Hyperglycemia Symptoms:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Headache
- Difficulty concentrating
What to Do:
- Check blood sugar to confirm elevation
- Drink water to stay hydrated
- Review recent food intake and activity
- Take prescribed medication if missed
- Exercise if blood sugar isn’t extremely high
- Contact healthcare provider if blood sugar remains elevated or if you feel very unwell
Diabetic Ketoacidosis (DKA): In Type 1 diabetes, very high blood sugar with insufficient insulin can lead to DKA, a life-threatening emergency. Symptoms include nausea, vomiting, abdominal pain, fruity-smelling breath, and rapid breathing. Seek immediate medical attention if these symptoms occur.
Hypoglycemia: Low Blood Sugar
Hypoglycemia occurs when blood sugar drops too low, typically below 70 mg/dL.
Hypoglycemia Symptoms:
- Shakiness or trembling
- Sweating
- Rapid heartbeat
- Hunger
- Dizziness or lightheadedness
- Confusion or difficulty concentrating
- Irritability or mood changes
- Pale skin
What to Do (Rule of 15):
- Check blood sugar to confirm it’s low
- Consume 15 grams of fast-acting carbohydrates (3-4 glucose tablets, 4 ounces juice, or 1 tablespoon honey)
- Wait 15 minutes
- Recheck blood sugar
- If still below 70 mg/dL, repeat treatment
- Once blood sugar normalizes, eat a small snack or meal to prevent recurrence
Severe Hypoglycemia: If blood sugar drops so low that you become confused, lose consciousness, or have seizures, this constitutes a medical emergency. Family members should know how to administer glucagon and when to call emergency services.
Preventing Blood Sugar Extremes
For Hyperglycemia Prevention:
- Take medications as prescribed
- Monitor carbohydrate intake
- Stay physically active
- Manage stress
- Stay hydrated
For Hypoglycemia Prevention:
- Don’t skip meals
- Match medication doses to food intake and activity
- Check blood sugar before driving or activities where low blood sugar could be dangerous
- Carry fast-acting carbohydrates always
- Wear medical identification indicating diabetes
Survival Tip 8: Build Your Diabetes Care Team
Living successfully with diabetes requires support. Building a strong healthcare team and support network provides the guidance, expertise, and encouragement needed for long-term success.
Your Healthcare Team
Comprehensive diabetes care involves multiple specialists:
Primary Care Physician or Endocrinologist: Oversees overall diabetes management, prescribes medications, and coordinates care. Regular visits ensure your treatment plan remains appropriate as circumstances change.
Diabetes Educator: Provides education about blood sugar monitoring, medication administration, nutrition, and lifestyle management. These specialists help you develop practical skills for daily diabetes management.
Dietitian: Offers personalized nutrition guidance considering your food preferences, lifestyle, and blood sugar patterns. Moreover, dietitians help with meal planning and problem-solving challenging nutrition situations.
Eye Doctor: Performs annual dilated eye examinations to detect diabetic retinopathy early.
Dentist: Provides regular dental care and treats gum disease, which affects diabetes control.
Podiatrist: Specializes in foot care, preventing and treating foot complications.
Mental Health Professional: Addresses stress, anxiety, depression, and diabetes burnout that commonly affect people with chronic conditions.
Family and Social Support
Beyond healthcare professionals, family and friends provide crucial support:
Educate Loved Ones: Help family members understand diabetes, including how to recognize and respond to blood sugar emergencies. Their understanding increases support effectiveness.
Communicate Needs: Express what kind of support helps you most. Some people want accountability partners for exercise or healthy eating, while others prefer emotional support without monitoring.
Join Support Groups: Connecting with others managing diabetes provides practical tips, emotional support, and reduces isolation. Both in-person and online support groups offer valuable connections.
Address Family Dynamics: Diabetes affects the entire family. Open communication about challenges and needs helps family members support rather than inadvertently undermine diabetes management.
Survival Tip 9: Stay Current with Diabetes Care
Diabetes management continues evolving with new medications, technologies, and treatment approaches constantly emerging. Therefore, staying informed helps you benefit from advances that improve control and quality of life.
Continuous Learning
Attend Diabetes Education Programs: Formal education programs provide comprehensive diabetes management training. Moreover, refresher courses update knowledge as guidelines change.
Follow Reputable Sources: Stay informed through trusted diabetes organizations rather than unreliable internet sources. Quality information helps you make sound decisions.
Ask Questions: Never hesitate to ask your healthcare team about new symptoms, treatment options, or management strategies. No question is too small when it affects your health.
Keep Records: Track blood sugar patterns, medications, diet, exercise, and how you feel. These records help you and your healthcare team identify patterns and optimize management.
Regular Health Screening
Consistent health screening remains vital for monitoring diabetes control and detecting complications early. Schedule regular appointments even when feeling well, as many diabetes complications develop silently.
Comprehensive screening should include:
- HbA1c testing every 3-6 months
- Annual kidney function testing
- Annual cholesterol panel
- Regular blood pressure monitoring
- Annual comprehensive eye examination
- Annual foot examination
HOP Medical Centre offers convenient health screening packages designed for people with diabetes, including all necessary tests to monitor control and detect complications early. Regular screening at our Orchard or Tampines locations ensures you stay on track with diabetes management.
Survival Tip 10: Practice Self-Advocacy
Taking active role in your diabetes care leads to better outcomes and greater satisfaction with management. Self-advocacy means speaking up for your needs, asking questions, and making informed decisions about your care.
Know Your Rights
As a person with diabetes, you have rights:
Right to Quality Care: You deserve competent, respectful healthcare from providers who take your concerns seriously.
Right to Information: You should receive clear explanations about your condition, treatment options, and expected outcomes.
Right to Participate in Decisions: Healthcare decisions should be made collaboratively, considering your preferences, values, and circumstances.
Right to Second Opinions: If uncertain about recommended treatment, seeking another perspective is completely appropriate.
Effective Communication with Healthcare Providers
Prepare for Appointments: Write down questions, concerns, and information to share before appointments. Bring blood sugar logs and medication lists.
Be Honest: Share challenges honestly rather than reporting only successes. Your healthcare team can’t help address problems they don’t know exist.
Ask for Clarification: If you don’t understand something, ask for explanation in terms you can understand. Good providers welcome questions.
Express Preferences: Share your goals, concerns, and what matters most to you. Management plans work better when they align with your priorities.
Follow Through: Implement agreed-upon plans and report back on results. This collaboration helps fine-tune management strategies.
Taking Control: Your Diabetes Survival Action Plan
Living well with diabetes requires daily attention and consistent effort. However, implementing these survival tips transforms diabetes from an overwhelming burden into a manageable condition that doesn’t prevent you from living fully.
Start by focusing on one or two tips that seem most relevant to your current situation. Gradually incorporate additional strategies as new habits become routine. Remember that perfection isn’t the goal—consistent effort over time produces results.
Regular health screening provides objective feedback about how well your survival strategies are working. Schedule comprehensive diabetes screening if you haven’t been tested recently or if your diabetes control seems suboptimal. Early detection of problems allows timely intervention that prevents serious complications.
Don’t face diabetes alone. Build your support team, connect with others managing diabetes, and lean on healthcare professionals for guidance. With the right knowledge, support, and daily commitment, you can not only survive with diabetes but thrive, enjoying active, fulfilling life while protecting your health for years to come.
Frequently Asked Questions About Diabetes Management
Can Type 2 diabetes be reversed?
While “cure” isn’t accurate, some people with Type 2 diabetes achieve remission through significant weight loss, improved diet, and increased physical activity. However, remission requires ongoing healthy lifestyle maintenance. Moreover, even with remission, continued monitoring remains important as diabetes can return.
How often should I check my blood sugar?
Frequency depends on diabetes type and treatment. People taking insulin typically check multiple times daily, while those managing Type 2 diabetes with diet or oral medications may check less frequently. Discuss appropriate monitoring schedule with your healthcare provider.
What’s the difference between blood sugar and HbA1c?
Blood sugar testing provides a snapshot of current glucose levels, while HbA1c shows average blood sugar over the previous 2-3 months. Both measurements provide valuable but different information about diabetes control.
Can I eat fruit with diabetes?
Yes, fruit can be part of a healthy diabetes diet. Whole fruits contain fiber, vitamins, and minerals. However, watch portions and balance fruit with other foods. Limit fruit juice, which lacks fiber and causes rapid blood sugar increases.
Should I avoid all carbohydrates?
No, you need carbohydrates for energy. Focus on choosing high-quality carbohydrates including whole grains, vegetables, legumes, and fruits, while limiting refined carbohydrates and added sugars. Moreover, portion control matters more than complete avoidance.
How can I prevent diabetes complications?
The most important prevention strategy is maintaining blood sugar, blood pressure, and cholesterol within target ranges. Additionally, don’t smoke, attend all recommended screening appointments, practice daily self-care, and address problems promptly when they arise.
What should I do if I miss a medication dose?
Generally, take the missed dose as soon as you remember unless it’s close to the next scheduled dose. Never double doses without medical guidance. Consult your healthcare provider or pharmacist for specific instructions regarding your medications.
Can stress really affect my blood sugar that much?
Yes, stress significantly impacts blood sugar through hormonal responses and behavioral changes. Many people notice their blood sugar runs higher during stressful periods. Therefore, stress management represents an important component of diabetes control.
Your Path Forward: Living Successfully with Diabetes
Diabetes requires daily attention, but it doesn’t have to control your life. The survival tips outlined in this guide provide a roadmap for managing diabetes effectively while maintaining quality of life. By monitoring blood sugar regularly, eating well, staying active, taking medications as prescribed, managing stress, preventing complications, recognizing blood sugar extremes, building support networks, staying informed, and advocating for yourself, you take control of diabetes rather than letting it control you.
Remember that diabetes management is a marathon, not a sprint. Some days will be easier than others, and that’s normal. What matters is consistent effort over time and getting back on track after challenging periods. Celebrate your successes, learn from difficulties, and keep moving forward with confidence that you can live well with diabetes.
Regular health screening remains essential for monitoring your progress and detecting problems early. If you haven’t had comprehensive diabetes screening recently, schedule an appointment to assess your current control and identify areas needing attention.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Diabetes management decisions should be made in consultation with qualified healthcare professionals who can assess your individual health status, medical history, and specific circumstances. Treatment recommendations vary based on diabetes type, complications presence, overall health, and personal factors. Always follow medical advice from your healthcare providers.
With over 20 years of trusted medical expertise in Singapore, comprehensive diagnostic capabilities including HbA1c testing and diabetes monitoring, and convenient locations in Orchard and Tampines, HOP Medical Centre provides quality diabetes screening and management support. Whether you need regular diabetes monitoring, complication screening, or initial diabetes assessment, our experienced medical team is committed to supporting your health through accurate diagnosis and professional care. Contact us today to schedule diabetes screening or explore our health screening packages that include comprehensive diabetes assessment for effective management and complication prevention.
